Background: Fluoroquinolones (FQL) are commonly used in antimicrobial prophylaxis in immunocompromised cancer patients (pts) during prolonged neutropenia. A possibly high and increasing proportion of pts harboring FQL-resistant Enterobacteriaceae (FRE) challenges the assumption that prophylaxis with FQLs is still of benefit in preventing sepsis. Previous studies reported that colonization of FRE in allogeneic transplant patients may be an infection risk factor (cf. Satlin et al. Clin Infect Dis 202;73:1257-65). This prospective study aims to determine the prevalence of FRE in defined pt populations in two metropolitan areas treated with dose-intense melphalan with autologous peripheral blood stem cell (PBSC) transplantation, and to determine the possible clinical effects of FRE in the host microbiome on transplant outcomes.
Methods: Pts eligible for this prospective, ongoing study have a diagnosis of MM and are undergoing autologous PBSC transplantation after conditioning with dose-intense melphalan 200 mg/m 2 at Hackensack University Medical Center (HUMC) and MedStar Georgetown University Hospital (MGUH). Peri-rectal swabs are scheduled before chemotherapy mobilization of PBSC given with FQL prophylaxis, before transplant admission with initiation of antimicrobial prophylaxis, at time of hospital discharge, and 3 months after aHSCT. Prophylaxis is discontinued with fever or hospital discharge. Blood cultures are obtained at time of fever (>38 °C) with adjustments in antibiotics per standard of care. A central catheter is placed for venous access in all patients throughout their transplant course. Pts are discharged after achieving neutrophil (ANC) engraftment and control of conditioning regimen toxicities. Bacterial cultures from perirectal swabs (fresh or frozen for shipping) were purified on CHROMagar™ Orientation Plates and grown in the presence of ≥5 ug/ml ciprofloxacin to select for quinolone-resistant organisms.
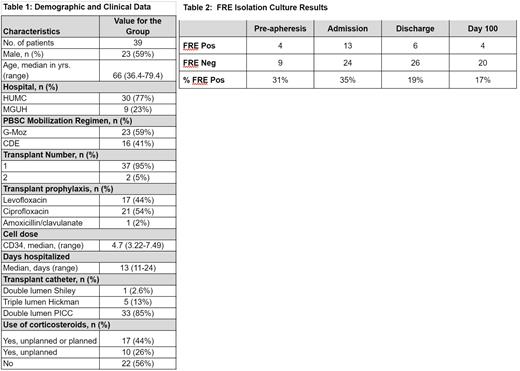
Results: To date, 39 pts are evaluable (Table 1). PBSC were mobilized using filgrastim/plerixafor (G-Moz) or cyclophosphamide/etoposide/dexamethasone (CDE) followed by filgrastim with levofloxacin prophylaxis. The quantity of CD34+ cells infused is in Table 1. All pts achieved ANC engraftment at a median of 10.8 days (range 9-14) and were hospitalized for a median of 13 days (range 11-24). 37/39 pts collected swabs before transplant admission (and swabs were obtained at discharge for the other 2 pts). 13/37 (35%) admission swabs demonstrated FRE colonization (Table 2). 6/33 swabs at time of discharge were positive for FRE including for 4 pts negative for FRE on transplant admission with a total of 17/39 pts (44%) showing FRE colonization at some point during the transplant admission. Samples collected at 3 months after transplantation for 24 pts reaching that timepoint showed FRE colonization for 4 pts including 2 pts not previously testing positive at time of transplantation. 27/107 samples tested positive for FRE and 21/39 pts (54%) had at least one FRE positive culture.
Seven pts (20%) developed neutropenic fever but no pt experienced a blood-stream infection (BSI). One pt developed Clostridium difficile colitis during the period of neutropenia. One pt tested positive for MRSA colonization at admission but did not develop fever or BSI. One pt was readmitted after initial hospital discharge for evaluation of fever without a source of infection determined. Ten pts (5 FRE colonized during transplant course) were given prednisone for persistent diarrhea attributed to engraftment syndrome (cf: Spitzer TR. Bone Marrow Transplant 2001;27:893-8) commencing at a median of 10 (range, 8-13) days after aHSCT and not associated with CDE mobilization or detection of FRE. Nineteen other patients, 8 of whom tested positive for FRE, did not receive corticosteroids for management of regimen-related toxicities (an additional 7 pts received preplanned corticosteroids starting at day +8). No center effect is yet evident.
Conclusions: FRE are detected in a high proportion of pts undergoing aHSCT in the treatment of MM. However, FQL prophylaxis is not associated with FRE BSI in this ongoing study. FRE colonization is not predictive of delayed engraftment or prolonged hospitalization, and does not appear predictive of non-infectious diarrhea.
Disclosures
Rowley:ReAlta Life Science: Consultancy; SIRPant Immunotherapeutics: Membership on an entity's Board of Directors or advisory committees. Renteria:Kymera Therapeutics: Consultancy; Novo Nordisk: Consultancy. Munshi:Kite, a Gilead company: Speakers Bureau; Incyte: Consultancy, Speakers Bureau. Suh:Kite Pharma: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal